
Taking a "whole person" approach to healthcare means addressing limitations that prevent individuals from getting the most effective care possible. Gaps in care can significantly impact a person's quality of life, the efficacy of provider-prescribed treatments, and have lasting financial implications.
This article examines the gaps in COPD care, demonstrates the importance of accounting for COPD in your roadmap, and discusses how Wellinks is addressing clinical needs for better patient outcomes and long-term cost savings.
Lived Patient Experience
When managed properly, it is possible to maintain a good quality of life while living with COPD. However, barriers exist to accessing effective care and treatment options, preventing a majority of the 16.4 million Americans* living with the disease from maintaining their well-being.
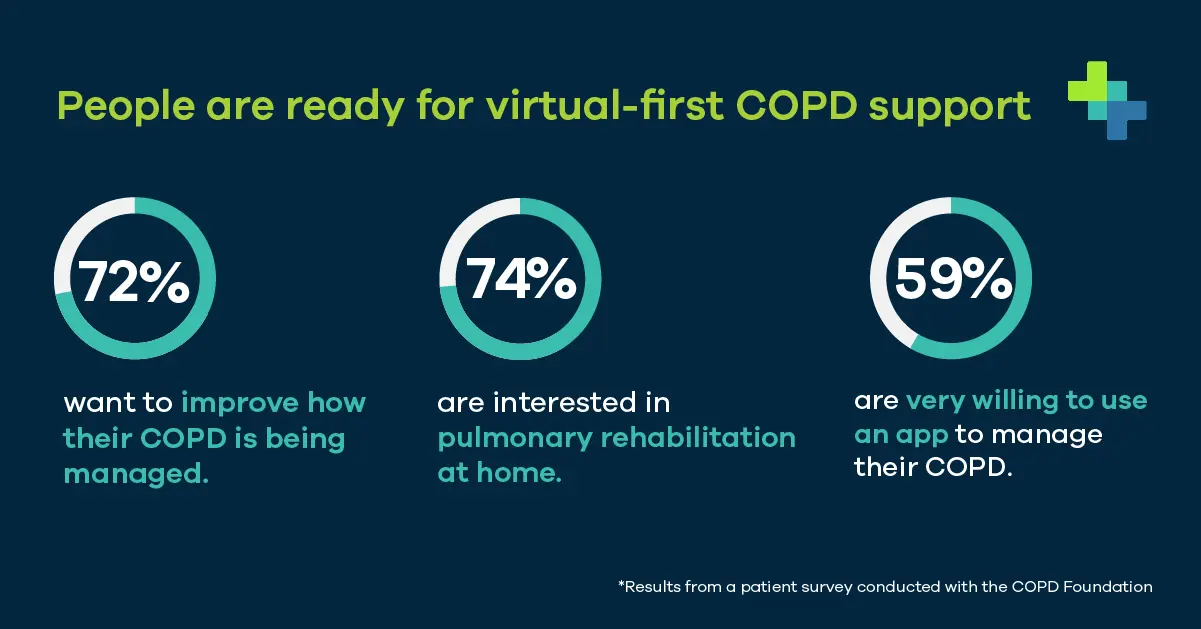
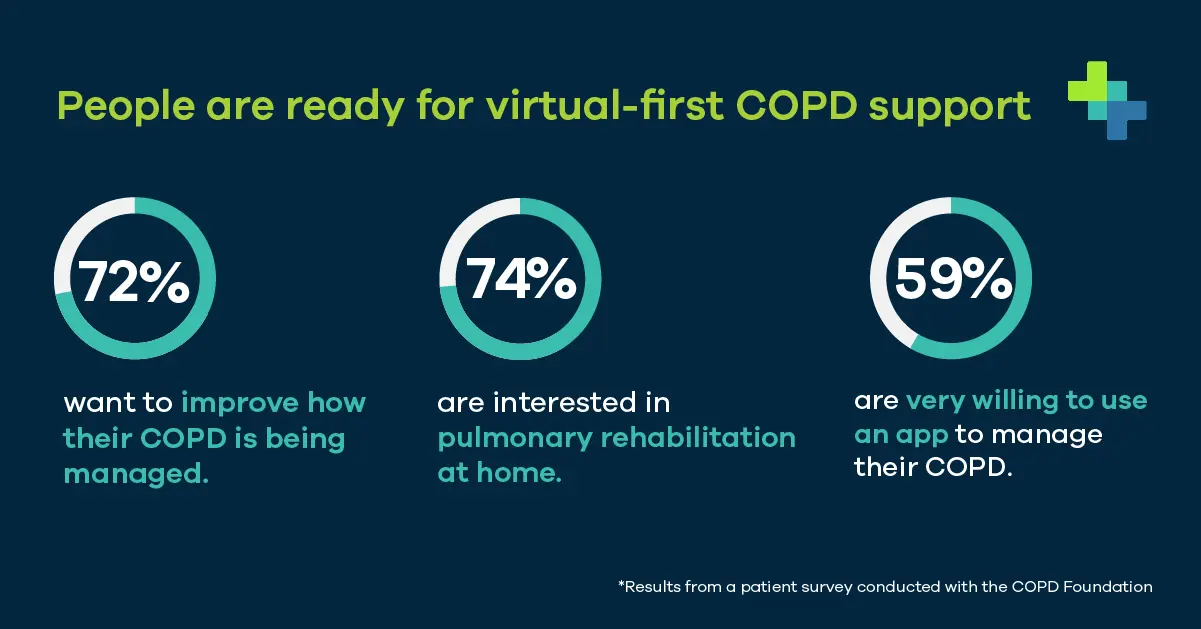
Wellinks, in collaboration with the COPD Foundation, conducted a survey to better understand the perspectives and experiences of people living with COPD in the United States. What we discovered was shocking.
Go Deeper: The Lived Experiences of People with COPD
Not only do these emergency visits and additional treatments negatively impact a person's physical and mental well-being, but they also rack up staggering medical debt. On average, individuals with COPD accumulate $6,246* more per year in medical costs than someone without COPD. The startling statistics bring to mind many questions, with the most critical being:
Lack of Access to Effective Care, Especially Pulmonary Rehabilitation
One of the most recommended and effective treatment options for people with COPD is Pulmonary rehabilitation (PR). Shockingly, less than 3%* of that population utilizes this therapy due to significant barriers and gaps.
From the provider side:
From the individual's standpoint:
A solution can be found in the large appetite that exists for more accessible, integrated, and virtual care options that meet people where they are. Virtual tools are essential as they can simplify the patient experience and overcome physical barriers limiting access to care. Our survey identified strong demand, and people with COPD are ready for change.
Wellinks integrated, virtual-first COPD management solution is resolving these gaps in care by increasing access to high-quality care outside of the doctor's office. Our connected devices give members the following:
Virtual solutions help individuals overcome the mental and physical barriers associated with COPD. Wellinks is actively addressing the gaps and barriers preventing individuals with COPD from obtaining better health and providers from offering critical support. Our approach has demonstrated increased levels of self-efficacy among members and has seen significant improvements in their quality of life.
Go Deeper: Member Testimonial: Meet Phyliss
Financial Impact & Solutions
From a financial standpoint, the need to address these gaps are critical. COPD is the 5th most costly chronic disease in the U.S. and has $49B in associated healthcare costs that are expected to grow to $800B in the next 20 years due to:
Moreover, a large portion of these costs can be attributed to in-patient management of exacerbations, including preventable ED visits and hospitalizations.
The financial burden COPD places on our healthcare industry can be reduced or avoided by educating patients on how to manage their COPD properly. Wellinks takes a proactive, whole-person approach to COPD care to improve patient outcomes and reduce medical expenses.
Go Deeper: Show me the Numbers
This approach is representative of the Value-Based Care (VBC) model and has the possibility to impact other diseases, thus lowering overall healthcare costs. While slowly being adopted across the healthcare industry, this model can significantly impact a disease like COPD as it is a progressive, non-curable disease with a history that demonstrates exacerbations create long-term deficits to a patient's health. Preventative care and avoiding exacerbations are techniques for managing this condition. However, it is essential to encourage self-efficacy and self-management for better patient results. PR is a vital piece in the puzzle for preventing the downward progression of those living with COPD, and the VBC model allows for more innovative approaches to disease management.
Go Deeper: AHIP Webinar
Working Towards Change
It is clear that the current system for COPD care is not working.
Individuals are not getting the care they need to manage their condition, and healthcare providers are overwhelmed and unable to meet the demand. The current approach to care is reactive, increasing costs on the individuals, providers, and payors. It's time for a change; "whole-person" care starts at the top. For patients, it's their quality of life which includes physical, mental, emotional, and financial health. For providers, it's their treatment plans' effectiveness and ability to give critical care where it's needed. For payors, it is the need to reduce costs wherever and whenever possible.
Wellinks is working to address significant gaps in COPD care. Contact us to learn how we can help improve outcomes and lower costs.
Subscribe to our newsletter and follow us on social media to stay up to date on the latest industry news and updates.
*SOURCES:
American Lung Association - COPD Trends Brief: Prevalence
National Library of Medicine - COPD Affects Worker Productivity and Health Care Costs
National Library of Medicine - The Need For Expanding Pulmonary Rehabilitation Services
JAMA Network - Cost-Effectiveness of Pulmonary Rehabilitation Among US Adults with COPD
Taking a "whole person" approach to healthcare means addressing limitations that prevent individuals from getting the most effective care possible. Gaps in care can significantly impact a person's quality of life, the efficacy of provider-prescribed treatments, and have lasting financial implications.
This article examines the gaps in COPD care, demonstrates the importance of accounting for COPD in your roadmap, and discusses how Wellinks is addressing clinical needs for better patient outcomes and long-term cost savings.
Lived Patient Experience
When managed properly, it is possible to maintain a good quality of life while living with COPD. However, barriers exist to accessing effective care and treatment options, preventing a majority of the 16.4 million Americans* living with the disease from maintaining their well-being.
Wellinks, in collaboration with the COPD Foundation, conducted a survey to better understand the perspectives and experiences of people living with COPD in the United States. What we discovered was shocking.
Go Deeper: The Lived Experiences of People with COPD
Not only do these emergency visits and additional treatments negatively impact a person's physical and mental well-being, but they also rack up staggering medical debt. On average, individuals with COPD accumulate $6,246* more per year in medical costs than someone without COPD. The startling statistics bring to mind many questions, with the most critical being:
Lack of Access to Effective Care, Especially Pulmonary Rehabilitation
One of the most recommended and effective treatment options for people with COPD is Pulmonary rehabilitation (PR). Shockingly, less than 3%* of that population utilizes this therapy due to significant barriers and gaps.
From the provider side:
From the individual's standpoint:
A solution can be found in the large appetite that exists for more accessible, integrated, and virtual care options that meet people where they are. Virtual tools are essential as they can simplify the patient experience and overcome physical barriers limiting access to care. Our survey identified strong demand, and people with COPD are ready for change.
Wellinks integrated, virtual-first COPD management solution is resolving these gaps in care by increasing access to high-quality care outside of the doctor's office. Our connected devices give members the following:
Virtual solutions help individuals overcome the mental and physical barriers associated with COPD. Wellinks is actively addressing the gaps and barriers preventing individuals with COPD from obtaining better health and providers from offering critical support. Our approach has demonstrated increased levels of self-efficacy among members and has seen significant improvements in their quality of life.
Go Deeper: Member Testimonial: Meet Phyliss
Financial Impact & Solutions
From a financial standpoint, the need to address these gaps are critical. COPD is the 5th most costly chronic disease in the U.S. and has $49B in associated healthcare costs that are expected to grow to $800B in the next 20 years due to:
Moreover, a large portion of these costs can be attributed to in-patient management of exacerbations, including preventable ED visits and hospitalizations.
The financial burden COPD places on our healthcare industry can be reduced or avoided by educating patients on how to manage their COPD properly. Wellinks takes a proactive, whole-person approach to COPD care to improve patient outcomes and reduce medical expenses.
Go Deeper: Show me the Numbers
This approach is representative of the Value-Based Care (VBC) model and has the possibility to impact other diseases, thus lowering overall healthcare costs. While slowly being adopted across the healthcare industry, this model can significantly impact a disease like COPD as it is a progressive, non-curable disease with a history that demonstrates exacerbations create long-term deficits to a patient's health. Preventative care and avoiding exacerbations are techniques for managing this condition. However, it is essential to encourage self-efficacy and self-management for better patient results. PR is a vital piece in the puzzle for preventing the downward progression of those living with COPD, and the VBC model allows for more innovative approaches to disease management.
Go Deeper: AHIP Webinar
Working Towards Change
It is clear that the current system for COPD care is not working.
Individuals are not getting the care they need to manage their condition, and healthcare providers are overwhelmed and unable to meet the demand. The current approach to care is reactive, increasing costs on the individuals, providers, and payors. It's time for a change; "whole-person" care starts at the top. For patients, it's their quality of life which includes physical, mental, emotional, and financial health. For providers, it's their treatment plans' effectiveness and ability to give critical care where it's needed. For payors, it is the need to reduce costs wherever and whenever possible.
Wellinks is working to address significant gaps in COPD care. Contact us to learn how we can help improve outcomes and lower costs.
Subscribe to our newsletter and follow us on social media to stay up to date on the latest industry news and updates.
*SOURCES:
American Lung Association - COPD Trends Brief: Prevalence
National Library of Medicine - COPD Affects Worker Productivity and Health Care Costs
National Library of Medicine - The Need For Expanding Pulmonary Rehabilitation Services
JAMA Network - Cost-Effectiveness of Pulmonary Rehabilitation Among US Adults with COPD